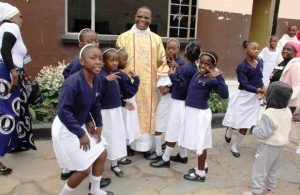
Started in a Comboni Parish Our Lady of Africa in Mbuya in the outskirts of Kampala, the ReachOut Ugandan Health Initiative has changed the lives of many people with HIV. We visited the project.
When you step through the doors of ReachOut Mbuya, you know you are somewhere special. The walls are lined with accreditations and awards. Everywhere are images of dignitaries from around the world who have come to learn of the work taking place here.
Most impressively, everyone is smiling. Smiles are not something easily identified with the AIDS crisis in Africa, but the employees and clients at ReachOut have a lot to smile about.
In 2001, Comboni Father Joseph Archetti recognised a new strain on the resources of his parish, Our Lady of Africa in the Mbuya neighbourhood of Kampala. Priests were being called in increasing numbers to anoint and minister to the dying. Many parishioners had contracted AIDS and Fr. Archetti began to wonder if the parish could do more than comfort the dying.
From a pilot project working out of a room in the church basement and serving fourteen clients, ReachOut has grown to more than 20,000 patients and supports more than 1,000 orphans. It has additional locations in Kampala and in the rural reaches of Uganda.
Father Paolino Mondo, current parish priest of Our Lady of Africa shared one of the secrets to ReachOut’s success – a cache of antiretroviral medications (ARVs) provided by the US Centres for Disease Control (CDC).
The medicine supply is more secure than a bank vault and ReachOut staff are meticulous in their record-keeping. While some charities have not been able to continue receiving shipments of ARVs (medical supplies are often subject to theft or mismanagement, bringing profit to outlaws rather than health to the patients), the CDC consistently lauds ReachOut’s performance as exemplary. In fact, HIV clinics in neighbouring countries have made visits to Mbuya to learn best practices for administering their own programs.
While security and diligence are important, ReachOut offers another important difference: a community-based approach to healthcare. Two decades ago in Uganda, an HIV positive diagnosis seemed like a death sentence and was certain to ostracize the patient.
In some areas, HIV was seen as a curse. So not only did a person have to cope with the bad news of diagnosis, they also often found themselves abandoned by their neighbours and families, with no one to care for their personal or medical needs. The result was that very few people were tested and HIV infection tore through the population.
ReachOut actively conducts campaigns encouraging HIV testing throughout the country and helps any who receive a diagnosis understand that HIV is treatable. Each patient is assigned a counsellor who explains the diagnosis, offers treatment options, and listens.
Crucially, many employees at ReachOut were once patients themselves. They know what it means to receive an HIV positive diagnosis, and they know the fear, shame, and struggle of seeking treatment.
For this reason, they are committed to eliminating the fear, shame, and struggle and focusing on the treatment. “When I have to visit someone to make sure they are taking their medication, I tell them my own story”, one worker told us. “It changes everything. They do not see me as an outsider who looks down on them, but as someone who was once where they are now and who is still alive, still working and making a positive contribution. It gives them great hope and helps them to continue with their treatment, even when it is difficult”.
The clinic is still on the grounds of the parish and now occupies a large, modern building and several smaller structures. People can be tested and receive counselling here. They can receive their medication. But there are other unexpected services as well— a mobile unit that takes medical staff, counsellors, and medication to those who are unable to visit; a Day-care Centre for children of patients (some of the children are patients themselves); and a mother and baby clinic that provides for the needs of pregnant women and their new-born infants —an especially vulnerable population.
Before the mother-and baby clinic, an HIV-positive woman expected that any children she might have would also test positive. Now, the majority of clients in the program who deliver have children that are HIV negative. All the services of ReachOut are provided to clients free of charge— an incredible achievement. However, every participant is required to help in their own recovery and treatment. “When someone tests positive, it does not affect just one person”, a counsellor said. “It affects the whole community. Who will care for the children or do the work when this person must visit the doctor or go for treatment? ReachOut treats the entire family, and that is how everyone gets better”.
– Kathleen M. Carroll